Dear Editor,
Cutaneous metastasis from lung adenocarcinoma is an unusual presenting symptom, occuring in 1% to 12%, and it is more prone to misdiagnosis, especially in women.1 Moreover, a mass that develops in a skin graft site where basal cell carcinoma (BCC) was previously removed is highly likely to be misdiagnosed as a hypertrophic scar or a recurrence of BCC. Herein, we report a rare metastatic lung adenocarcinoma of the scalp that developed in a twenty-year-old skin graft site of BCC.
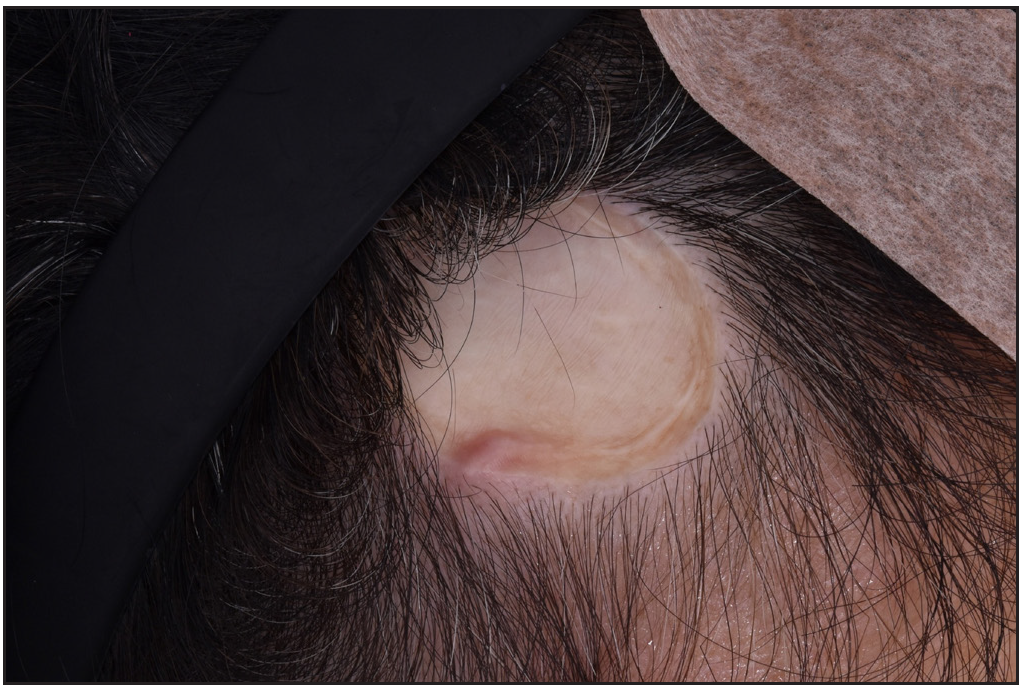
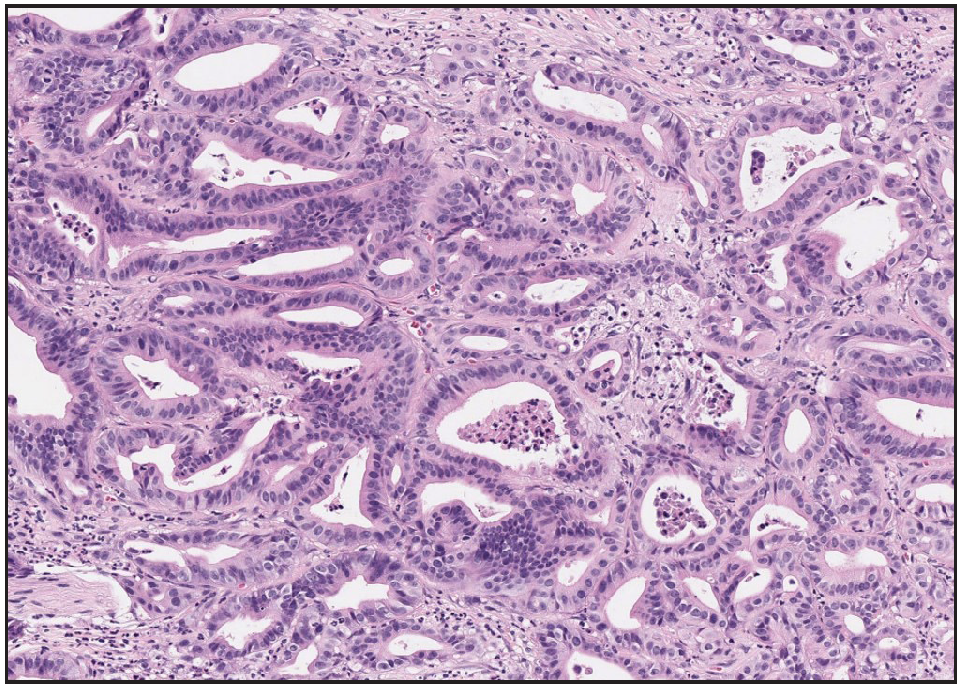
A 71-year-old woman presented with a skin-coloured solitary nodule on the scalp of 2-weeks duration [Figure 1]. She was diagnosed with lung adenocarcinoma three months prior and underwent a staging workup. Interestingly, the nodule developed where a split-thickness skin graft (STSG) surgery was performed for BCC twenty years ago. The donor site of the STSG was the right anterolateral thigh, and the surgical wound of the thigh had healed well. Initially, we suspected a hypertrophic scar after surgery or a recurrence of previous BCC. Skin biopsy from the scalp nodule revealed a poorly circumscribed infiltrating tumour with atypical epithelioid cells and gland like structures [Figure 2]. The immunohistochemistry test for thyroid transcription factor-1 showed a negative result. Based on the pathology findings, the patient was diagnosed with cutaneous metastatic adenocarcinoma arising from lung adenocarcinoma. Before the skin biopsy, a PET/CT scan hinted at the possibility of lung cancer that might not have spread to other parts of the body. However, following the skin biopsy, which confirmed metastasis, the patient’s diagnosis was revised to stage IVA.
Export to PPT
Export to PPT
In the case of skin metastasis with an unknown primary site, it is important to consider a wide-range of differential diagnoses.2 There are a few reported cases of metastatic adenocarcinoma in old scars.3 Among them, cutaneous metastasis from colonic adenocarcinoma in an old operative scar, such as a hysterectomy scar on the abdomen, is the most common, with direct implantation as a possible mechanism.4 Our case differs from previous reports as it involves metastatic lung adenocarcinoma.
The exact pathogenesis of cutaneous metastasis in old operative scars remains unclear. A possible mechanism includes the haematogenous spread of lung tumour cells rather than direct implantation.5 The alteration in the microscopic anatomy around the scar due to an altered adhesion molecule profile or altered local immunosurveillance mechanism may also contribute to the predilection for metastatic deposits on the old operative scars.3 In addition, owing to the increased scalp vasculature, the haematogenous route may be the more likely option for cutaneous metastasis to that site.6
We believe this exceptional presentation should prompt the inclusion of cutaneous metastasis in the differential diagnosis of masses that occur at a skin graft site, in addition to tumour recurrence. Furthermore, BCC exhibits a high recurrence rate, primarily linked to incomplete surgical resection.7 To validate our findings, further investigations are required.
Comments (0)